More often than not, Psychotherapy is thought to be useful for mentally ill patients. Hence, you might be surprised to know that Cognitive Behavioural Therapy (CBT), a tool of Psychotherapy, is widely used as a part of treatment for chronic diseases such as diabetes and cancer. The therapy positively impacts the patient’s quality of life and is often considered alongside regular medications.
Lauren Bell, a Cognitive Behavioural Therapist with the NHS, explains briefly what the therapy is, how it works, who benefits from it, and how is it useful for people with chronic diseases.
What is Cognitive Behavioral Therapy?
Cognitive Behavioural Therapy (CBT) is an evidence-based form of psychotherapy that looks at how we think, feel and behave. An effective treatment for a range of common mental health problems, NICE guidance recommends it.
CBT aims to empower patients by teaching them how to understand and then overcome their problems. It is a proven treatment method and is effective in treating and managing comorbid long-term physical health conditions. Besides, it is a highly collaborative treatment, with the ultimate aim of making patients their own therapists.
Could you help understand what types of long-term health conditions CBT can be most beneficial for?
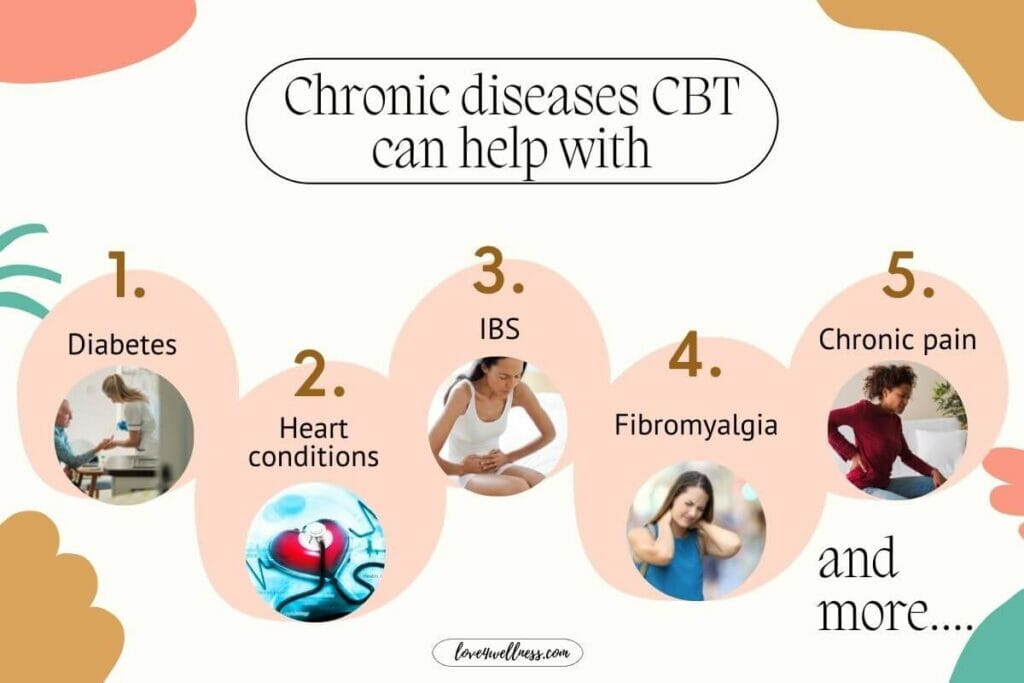
Cognitive Behavioural Therapy can help people manage comorbid long term health conditions such as diabetes, IBS, Heart conditions, Fibromyalgia, and Chronic pain. Study based evidence shows that people experiencing mental health difficulties alongside physical health conditions often have a significantly reduced quality of life. CBT aims to help them manage the overlap between their physical and mental health when suffering from chronic diseases.
How does CBT help those who suffer from chronic ailments? What is the possible outcome of undergoing CBT for chronic diseases?
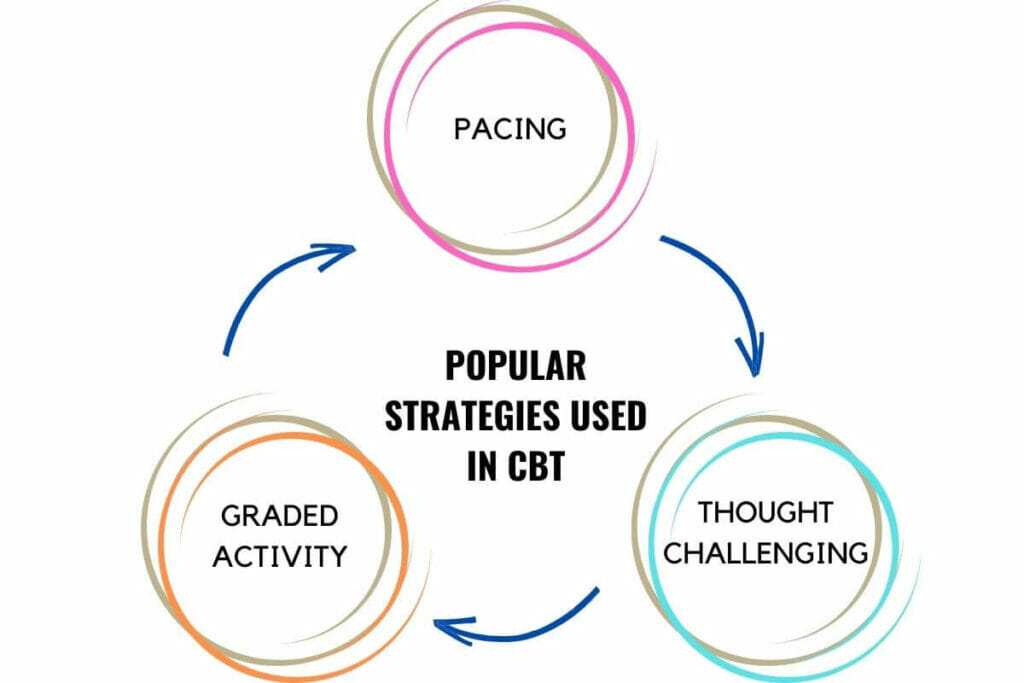
CBT for long term conditions addresses the overlap between physical and mental health. It helps to educate patients on how their physical and emotional states interact and teaches them strategies such as pacing, thought challenging and graded activity to allow them to gain better control of their mental and physical well-being.
People undergoing CBT for chronic health conditions can expect to feel an improvement in their emotional well-being, greater feelings of control over their physical health condition and improvements in health-related symptoms such as pain and discomfort.
What would the therapy sessions be like?
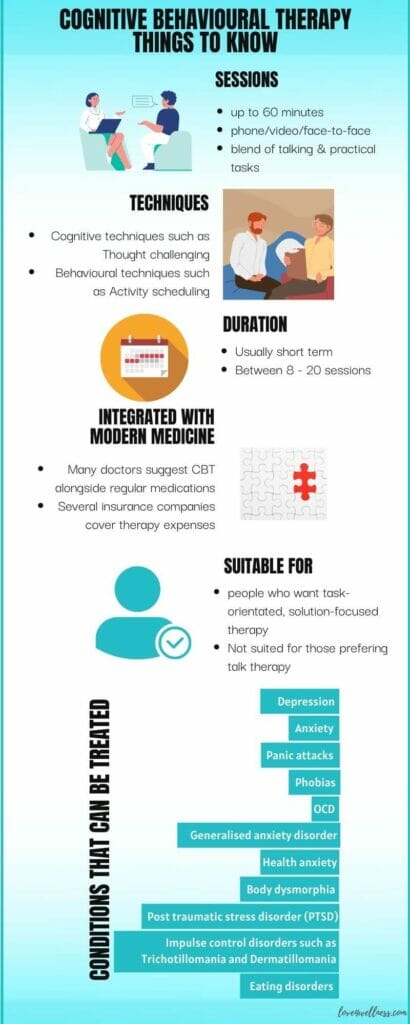
Therapy sessions are usually up to 60 minutes in duration and held over the phone, via video link or face-face. The therapist carefully tailors the sessions to each patient and will often contain adaptations such as pacing breaks to allow patients to manage their physical condition. Sessions are very collaborative and will have a blend of talking and practical, skills-based tasks. Patients are usually sent away with ‘homework’ to complete in between sessions, allowing them to build upon or consolidate learning.
What kinds of treatment modalities/approaches can one expect in the therapy process?
This all depends on what difficulties the person is presenting with. After an assessment, the first step of treatment is to develop a collaborative ‘formulation’. Such mapping of the problem helps both the patient and the therapist understand the problems and develop a treatment plan.
CBT uses a blend of ‘cognitive’ and ‘behavioural’ techniques. For instance, thought challenging is a popular cognitive technique. This aims to help the patient recognise negative thinking patterns and then challenge thoughts to promote balanced thinking. And a common behavioural strategy is ‘activity scheduling’ that aims to help patients see links between behaviour and mood and plan positive behavioural changes.
How long does the therapy last to show significant improvement in the patient?
CBT is a ‘short term’ therapy, and evidence suggests that anything from 8-20 sessions can be highly effective in promoting physical and mental health improvement.
How aware are people about CBT? Is CBT therapy integrated into modern medicine?
CBT is not a new therapy, but awareness of this type of Psychotherapy has definitely increased over recent years. This awareness has partly been thanks to the government IAPT (Improving Access to Psychological Therapies) initiative in the UK, which began in 2008.
And, yes, many doctors consider using CBT along with modern medicine, especially for people with chronic diseases. In fact, NICE recommends CBT as the treatment of choice for a number of common mental health problems such as Depression, and many doctors use CBT as a stand-alone treatment or alongside psychopharmacology.
Will insurance cover the therapy expenses?
This depends on the insurer and the policy held. Many insurers do now provide access to Psychological therapy as part of their package. Also, you can access the therapy for free through the NHS via local IAPT services. If you are not in the UK and live elsewhere, you can check with your local insurers and hospitals.
Is there a section of people to whom CBT will not be helpful?
CBT is quite an interactive treatment, so it works best for people who want a task-orientated, solution-focused form of therapy. However, CBT isn’t always helpful for those who prefer a more ‘pure talking’ therapy approach that other modalities such as counselling offers. CBT also works best for people who are able to recognise their own thoughts, feelings and behaviours and may feel a little tricky for people who struggle to identify these.
Can you share patient stories/testimonials/comments if possible(even anonymous ones will do, the intent is to provide an idea of what one might expect from the therapy)
Patient KM is a white 21-year-old British male. Unemployed, he lived at home with his mother. He presented for treatment after experiencing long term pain due to a shoulder break which would not heal.
KM was spending most of his day at home with curtains shut and presented with high levels of Depression. He reported feeling ‘not listened to’ by health professionals and was struggling to obtain a diagnosis.
KM engaged in CBT, and sessions initially focused on giving him an understanding of the crossover between his Pain and Depression. Planned strategies helped lift his mood and increase his physical activity levels. As a result, levels of pain improved. He was then taught to challenge his negative thoughts. He was also encouraged to engage in behavioural experiments to test out his negative predictions about certain activities.
The outcome of CBT was that the KM reported a significant reduction in Depression alongside improved pain levels and a better quality of life. He also felt able to begin searching for work due to improved confidence levels.
In your experience, what are the other areas where CBT can be highly beneficial apart from dealing with chronic diseases?
With several kinds of research happening on CBT as we speak, it is an effective form of therapy that treats a range of common mental health problems and conditions that include but not limited to:
- Depression
- Anxiety
- Panic Attacks
- Phobias
- OCD
- Generalised Anxiety Disorder
- Health Anxiety
- Body Dysmorphia
- Post Traumatic Stress Disorder
- Impulse control disorders such as Trichotillomania and Dermatillomania
- Eating disorders
The skills taught in CBT are universal and can be used by a range of people to treat a range of conditions. Besides, one can use the techniques taught repeatedly as part of a long term management strategy.
To conclude,
CBT is beneficial for the young and the old going through a painful phase during or after the treatment for chronic disease. As Lauren observes, there is more awareness about psychotherapy now than ever. Also, most hospitals have psychotherapy integrated into various treatments. So, when it is possible to reach out to a CBT therapist, please do so to reduce your distress and improve the quality of your life.
Edited by love4wellness | Images: canva.com