Please read this important disclaimer: This blog post provides general information about menopause symptoms and potential treatments. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Do not attempt to self-treat based on the information provided herein. Your healthcare provider can help you determine the most appropriate and safe treatment plan for your individual needs.
Menopause is a natural and inevitable phase in a woman’s life, signalling the end of her reproductive years. While it’s a universal experience, the journey through perimenopause (the years leading up to menopause) and postmenopause can vary significantly. Some women navigate this transition with minimal disruption, while others experience a range of symptoms that can impact their daily lives and overall well-being.
The good news is that there are numerous effective treatments available to help manage menopause symptoms, allowing women to embrace this new chapter with greater comfort and confidence.
This article aims to provide clear and simple information about the various treatments available for specific menopause symptoms, empowering every woman to make informed decisions about her care.
Understanding Menopause and Common Symptoms:
Menopause officially occurs when a woman has gone 12 consecutive months without a menstrual period, typically between the ages of 45 and 55. This happens because the ovaries gradually stop producing estrogen and progesterone. The fluctuating and declining levels of these hormones are responsible for the array of symptoms women may experience, including:
- Hot flashes and night sweats
- Irregular periods
- Vaginal dryness
- Sleep problems
- Mood changes (irritability, anxiety, depression)
- Urinary issues
- Changes in libido
- Joint pain and muscle aches
It’s important to remember that not every woman will experience all of these symptoms, and the intensity can vary greatly. Understanding which symptoms are most bothersome is the first step towards finding effective relief.
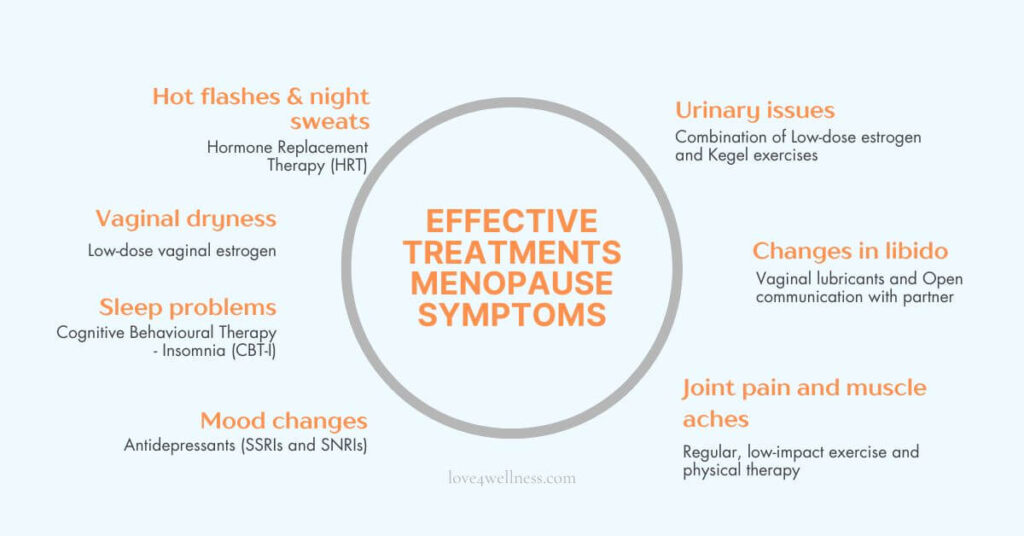
Targeting specific menopause symptoms with effective treatments:
Let’s delve into specific menopause symptoms and the treatments that can provide relief:
1. Vasomotor symptoms (Hot flashes and night sweats)
Hot flashes—those sudden waves of heat often followed by sweating and flushing—are one of the most common menopause symptoms. When they happen during sleep, they’re called night sweats and can seriously disrupt rest.
- Hormone replacement therapy (HRT): The gold standard for relieving hot flashes. It involves taking estrogen (with progestin if you have a uterus) to help regulate your body’s temperature control system. You can take it as a pill, patch, gel, or spray—your doctor can help you choose what works best for you.
- Non-hormonal medications: For women who cannot or choose not to take HRT, several non-hormonal medications can help.
- SSRIs and SNRIs (Selective Serotonin and Serotonin-Norepinephrine Reuptake Inhibitors): Certain antidepressants like paroxetine, venlafaxine, and escitalopram have been shown to reduce hot flash frequency, even in women without depression. They are believed to affect neurotransmitters that play a role in temperature regulation.
- Gabapentin and Pregabalin: These medications, primarily used for nerve pain and seizures, can also be effective in reducing hot flashes in some women.
- Clonidine: This blood pressure medication can offer mild relief from hot flashes for some individuals.
- Fezolinetant: This newer, non-hormonal medication specifically targets the brain’s temperature control centre and has shown significant promise in reducing the frequency and severity of moderate to severe hot flashes.
- Lifestyle changes:
- Dress in layers for quick cooling.
- Use fans, keep your bedroom cool, and take cool showers.
- Avoid triggers like spicy foods, caffeine, and alcohol.
- Try deep breathing or mindfulness to manage stress and reduce frequency.
Key Treatment Highlight: For significant relief from hot flashes and night sweats, Hormone Replacement Therapy (HRT), particularly systemic estrogen, is often the most effective option.
2. Vaginal dryness:
The decrease in estrogen can lead to thinning and drying of the vaginal tissues, causing discomfort, itching, and pain during sex.
- Low-dose vaginal estrogen: This is a highly effective treatment that directly addresses the issue. Available as creams, tablets, or vaginal rings, it delivers a small amount of estrogen directly to the vaginal tissues, improving moisture and elasticity with minimal systemic absorption.
- Non-hormonal options:
- Over-the-counter vaginal moisturisers used regularly can help maintain moisture.
- Water-based lubricants used during sexual activity can also alleviate discomfort.
- Avoid petroleum-based products as they can be irritating.
- Systemic HRT: Systemic HRT is primarily used for broader menopause symptoms, but it can also help with vaginal dryness. For this specific concern, local estrogen treatments are usually more effective and have fewer effects on the rest of the body.
Key Treatment Highlight: The most targeted and often effective treatment for vaginal dryness is Low-Dose Vaginal Estrogen.
3. Sleep problems (Insomnia, Difficulty staying asleep)
Hormonal changes can disrupt sleep patterns, making it hard to fall or stay asleep, or leaving you feeling unrested.
- Hormone therapy: By stabilising hormone levels, HRT can improve sleep for some women whose sleep disturbances are directly linked to hot flashes or hormonal imbalances.
- Non-hormonal medications: Certain antidepressants with sedative effects (taken at a low dose) may help with sleep. Other sleep medications might be prescribed cautiously for short-term use.
- Cognitive Behavioural Therapy for Insomnia (CBT-I): This therapy focuses on changing sleep habits and addressing underlying thoughts and behaviours that contribute to insomnia. It’s a highly effective long-term solution.
- Lifestyle changes:
- Keep a regular bedtime.
- Create a calming nighttime routine.
- Avoid screens, caffeine, and alcohol before bed.
- Make your bedroom dark, quiet, and cool.
- Get regular exercise, but not too close to bedtime.
Key Treatment Highlight: Cognitive Behavioural Therapy for Insomnia (CBT-I) is a highly recommended, non-pharmacological approach for long-term improvement in sleep.
4. Mood changes (Irritability, Anxiety, Depression)
Menopause can amplify emotional ups and downs, causing increased irritability, anxiety, or even depression.
- Hormone therapy: Estrogen can have a stabilising effect on mood for some women. If mood symptoms are significant, discussing HRT with a healthcare provider is important.
- Antidepressants (SSRIs/SNRIs): These medications are effective in treating menopause-related depression and anxiety, even in women who don’t have a history of these conditions.
- Cognitive Behavioural Therapy (CBT) and Mindfulness-based stress reduction (MBSR): These therapies can provide valuable tools for managing mood fluctuations, anxiety, and stress. CBT helps identify and change negative thought patterns, while MBSR focuses on present moment awareness and acceptance.
- Lifestyle changes:
- Exercise regularly to boost mood and energy.
- Eat a balanced diet rich in brain-healthy nutrients.
- Stay connected with friends and loved ones.
- Practice relaxation techniques like yoga or meditation.
Key Treatment Highlight: Antidepressants (SSRIs or SNRIs) can be very effective in managing menopause-related mood disorders.
5. Urinary issues (Incontinence, Increased UTIs)
Lower estrogen levels can weaken the tissues of the urethra and bladder, leading to urinary urgency, frequency, and incontinence, as well as an increased risk of urinary tract infections.
- Low-dose vaginal estrogen: By strengthening the vaginal and urethral tissues, local estrogen therapy can help improve urinary symptoms and reduce the risk of UTIs.
- Pelvic floor exercises (Kegels): Strengthening the pelvic floor muscles can improve bladder control and reduce incontinence.
- Lifestyle changes:
- Maintain adequate hydration.
- Avoid bladder irritants like caffeine and alcohol.
- Practising timed voiding (urinating at regular intervals) and double voiding (waiting a few minutes after urinating and then trying again) can be helpful.
Key Treatment Highlight: A combination of Low-Dose Vaginal Estrogen and Pelvic Floor Exercises (Kegels) is often the most effective approach for urinary issues.
6. Changes in libido
Lower estrogen levels, and sometimes lower testosterone too, can reduce your sex drive. Additionally, vaginal dryness can make sex uncomfortable, which can further decrease your desire.
- Hormone therapy: Systemic HRT, particularly estrogen combined with testosterone in some cases, may help improve libido. However, testosterone therapy for women is more complex and requires careful consideration and monitoring by a healthcare provider.
- Non-hormonal options:
- Addressing vaginal dryness with lubricants is crucial.
- Open and honest communication with your partner about changes in libido and exploring different forms of intimacy can be helpful.
- Addressing underlying mood issues or relationship problems can also positively impact libido.
Key Treatment Highlight: Addressing underlying causes like vaginal dryness with local estrogen and fostering open communication with a partner are key first steps.
7. Joint pain and muscle aches
Some women experience increased joint pain and muscle aches during menopause, possibly due to the decline in estrogen, which plays a role in reducing inflammation.
- Hormone therapy: For some women, HRT may help relieve joint pain, although it’s not a primary treatment for this symptom.
- Non-hormonal pain relievers: Over-the-counter pain relievers like ibuprofen or naproxen can help manage mild to moderate pain. Prescription pain medications may be necessary in some cases.
- Physical therapy and exercise: Maintaining muscle strength and flexibility through regular exercise, including low-impact options like swimming or walking, is crucial for managing joint pain. Physical therapy can also provide targeted exercises and pain management strategies.
- Weight management: Excess weight can put additional stress on joints, so maintaining a healthy weight is important.
Key Treatment Highlight: Regular, low-impact exercise and Physical Therapy are crucial for long-term management of joint pain and muscle aches.
Also Read: Arthritis Pain Relief | 6 Amazing Natural Remedies You Must Try
A note on natural remedies
Many women turn to natural and holistic methods, often inspired by ancient systems like Ayurveda and Traditional Chinese Medicine (TCM), to ease menopause symptoms.
- Phytoestrogens (in soy, flaxseed, lentils) may offer mild relief for hot flashes, though evidence is mixed. TCM sees these as nourishing for Yin, which declines during menopause.
- Herbal Remedies:
- Black Cohosh and Red Clover are commonly used for hot flashes, but research is inconclusive.
- Evening Primrose Oil is used for general women’s health, though evidence is limited.
- Ayurveda may suggest herbs like Shatavari, while TCM offers formulas to balance internal energy.
- Acupuncture may help reduce hot flashes and improve sleep by promoting energy flow, though results vary.
- Yoga and Meditation can support emotional well-being. Further, it can enhance sleep and relieve stress.
- Other Therapies like massage, aromatherapy, and homeopathy are also used, but lack strong scientific backing.
Note: These approaches may offer gentle support, but quality and safety can vary. It’s always best to talk to your doctor before trying any natural remedies.
Let’s sum it up
Menopause is a unique experience for every woman, and the symptoms can be diverse and sometimes challenging. However, a wide range of effective treatments is available, tailored to address specific symptoms and individual needs. From the well-established benefits of hormone therapy to the growing array of non-hormonal medications, lifestyle adjustments, and targeted therapies, women don’t have to suffer in silence.
The most important step is to have an open and honest conversation with your healthcare provider. They can accurately diagnose your symptoms, discuss your medical history and preferences, and thus help you develop an individualised treatment plan that will empower you to navigate menopause with greater ease and maintain a vibrant, fulfilling life. Remember, you are not alone, and effective help is available.
Images: canva.com